
Hodgkin’s Diseaseof the Lungs
Hodgkin’s Diseaseof the Lungs
© William Herring, MD, FACR

Hodgkin’s DiseaseGeneral Appearance
50% have mediastinal lymph nodeenlargement visible on chest x-ray
5-10% may have mediastinal adenopathywithout any other nodes involved

Hodgkin’s Disease
Clinically, over 90% have enlarged nodes
Disease behaves most benignly when restrictedto neck
Hodgkin’s more common to involve lungthan Non-Hodgkin’s Lymphoma

Hodgkin’s DiseasePatterns of Disease
Adenopathy
Parenchymal disease
Consolidation
Nodules
Atelectasis
Lymphangitic spread
Pleural effusion

Hodgkin’s DiseaseAdenopathy
Anterior mediastinal nodes commonlyinvolved
Paratracheal and para-aortic most common
Then hilar and subcarinal nodes
Hilar adenopathy usually bilateral butasymmetric
Internal mammary and posteriormediastinal nodes rare

Mediastinal adenopathy


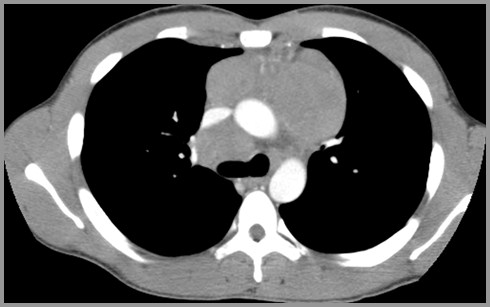
Mediastinal adenopathy

Hodgkin’s DiseaseParenchymal Involvement
Parenchymal involvement in 1/3
Almost all have associated hilar ormediastinal adenopathy
Except in recurrent disease
When unilateral, ipsilateral hilar adenopathy
Most have nodular sclerosing type

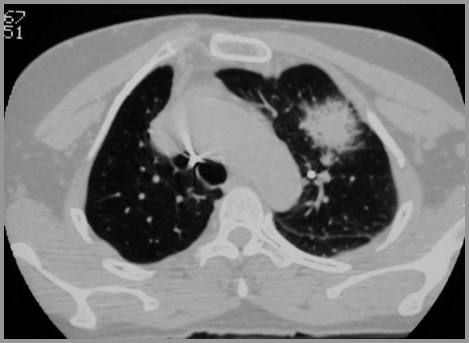
Parenchymal involvement in Hodgkin’sDisease

Hodgkin’s DiseaseConsolidation
Most commonly involves lung by directextension from hila
Air bronchograms frequently present
DDX: Alveolar cell ca and sarcoid

Parenchymal lymphoma with airbronchograms


Hodgkin’s DiseaseNodules
Less dense and less defined than BrCa
Usually single or few in number

Hodgkin’s DiseaseAtelectasis
Very uncommon
Almost always due to an endobronchiallesion
Rarely by compression

Hodgkin’s DiseasePleural Disease
About 1/3 have pleural effusions
Usually does not contain malignant cells

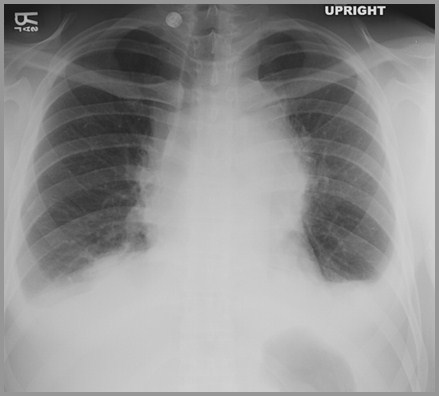
Massive mediastinal adenopathy andbilateral pleural effusions (yellow arrows)

Hodgkin’s DiseaseLymphangitic Spread
Least common parenchymal manifestation
Other causes should be sought
CHF
Allergic reaction
Infection

Hodgkin’s DiseasePrognosis
Mediastinal node enlargement worsensprognosis but only minimally
Diffuse lung involvement carries graveprognosis

Hodgkin’s DiseaseX-Ray Therapy
Thoracic XRT portal is called “mantel”because of T shape to coversupraclavicular and mediastinal nodes
Lymphoma is radiosensitive
Tumors frequently begin to show reduction insize almost at once
May calcify after radiation therapy

Calcification in treated anterior mediastinallymph nodes

Hodgkin’s DiseaseStage I and Stage II
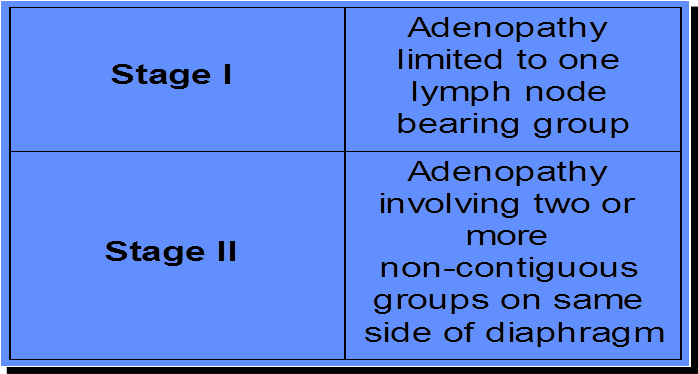

Hodgkin’s DiseaseStage III and Stage IV
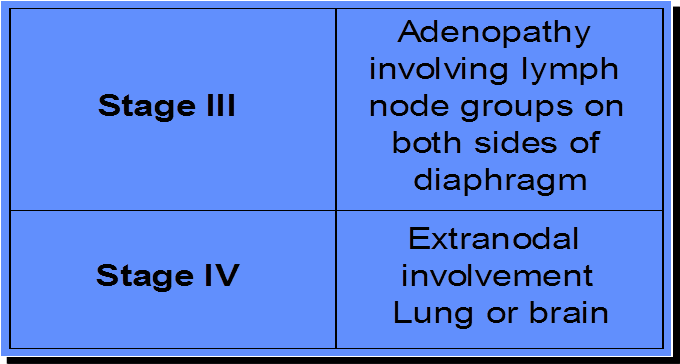

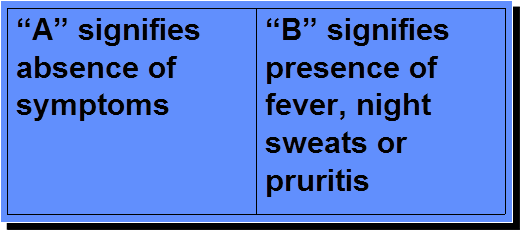
Hodgkin’s DiseaseAsymptomatic vs. Symptomatic

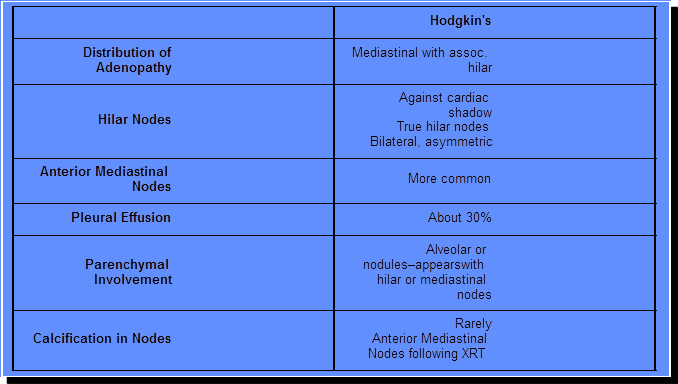
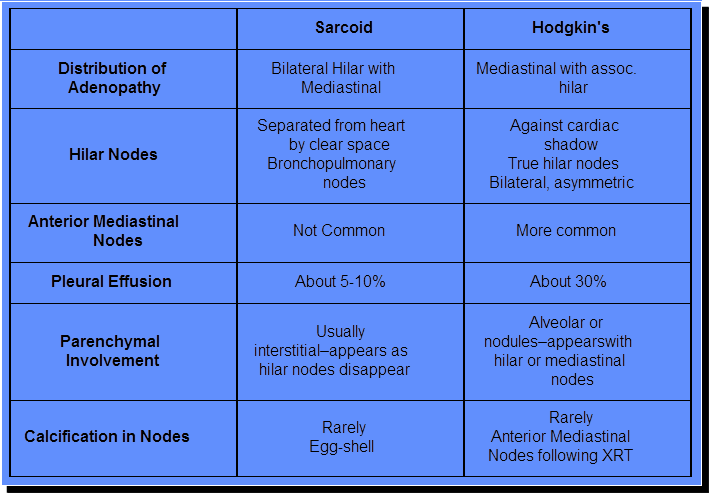
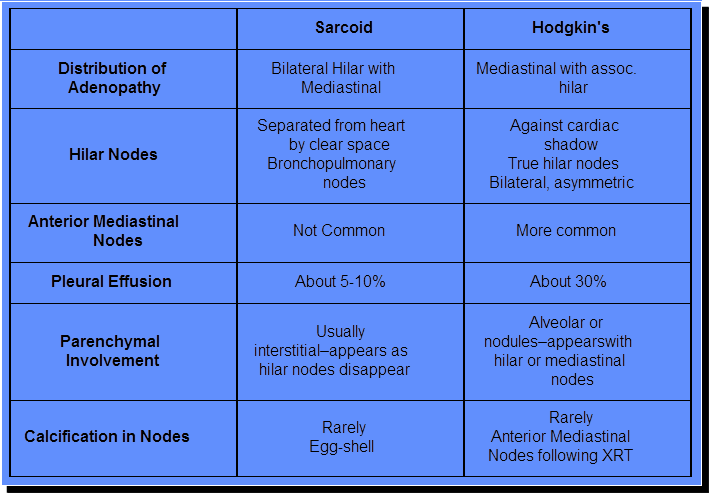
Hodgkin’s vs. Sarcoid
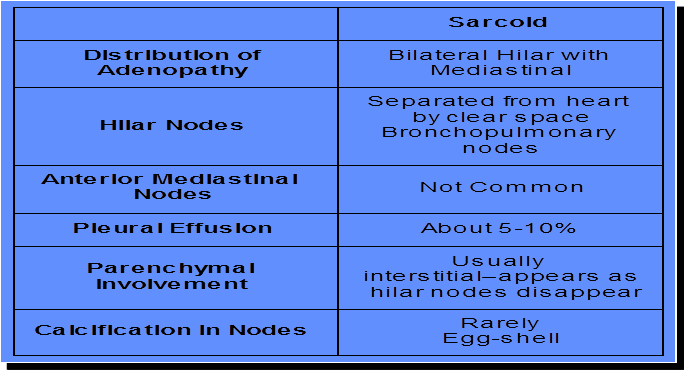

Hodgkin’s vs. Sarcoid





Non-Hodgkin’s Lymphoma(NHL) of the Lungs
Non-Hodgkin’s Lymphoma(NHL) of the Lungs

Non-Hodgkin’s Lymphoma
Primary NHL of the lungs is rare
Less than .4% of all lymphomas
Equal in males and females
Median age 55 years
May be identical to pseudolymphomaaccording to many authors

Non-Hodgkin’s LymphomaPathological
Divided into small cell lymphoma
More common
More often have pulmonary disease
Large cell (histiocytic) type
More often have hilar and mediastinal nodes

Non-Hodgkin’s LymphomaX-Ray Patterns
Reticulonodular
Most common form of NHL-looks likelymphangitic carcinoma
Nodular
Usually multiple and large
Almost never cavitate
Parenchymal consolidation
“Mass” with air bronchogram (DDX:Alveolar cell ca, sarcoid)
Miliary pattern

Non-Hodgkin’s LymphomaX-Ray
Predilection to cross fissures
Masses tend to undergo extremely rapidchange in size mimicking pneumonia
Effusions in fewer than a third (less thanHodgkin’s) and usually late in disease

Non-Hodgkin’s LymphomaPrognosis
Small cell lymphoma has good prognosis
Large cell lymphoma has worse prognosis

Castleman’s Disease
Giant Lymph Node Hyperplasia
Angiofollicular lymph node hyperplasia

Castleman’s Disease
Rare
Occurs in young adults
Two pathologic types
Hyaline vascular type
More common
Plasma cell type

Castleman’s Disease
Solitary mass of nodes usually in middleor posterior mediastinum
May be hypervascular on angio orcontrast enhanced CT
Good prognosis

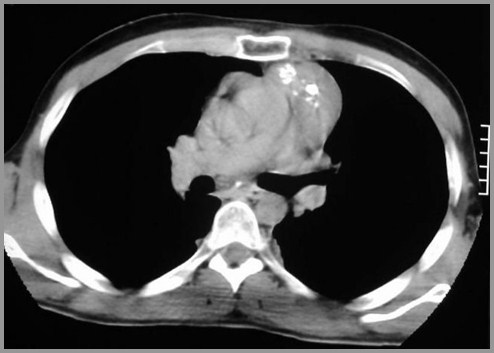
Solitary mass of nodes in Castleman’s Disease


The End